Saving lives in record time

Summary
Asante's STEMI program is a national leader in treating patients with a blocked artery to the heart.
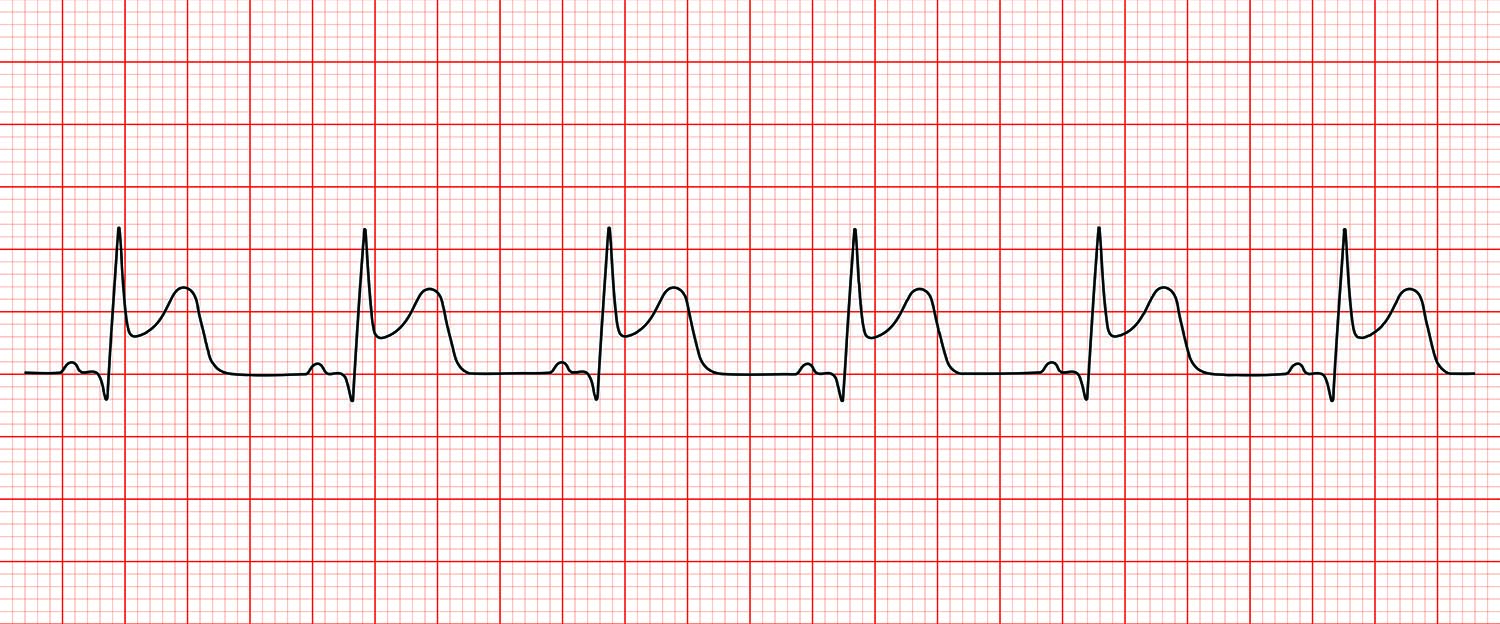
The STEMI (ST Segment Elevation Myocardial Infarction) program simultaneously activates paramedics, emergency departments and Asante Rogue Regional’s cath lab to rapidly identify and treat STEMIs throughout Southern Oregon and Northern California.
The program has received ongoing national recognition for its dramatic reduction in death rates from heart attacks — from about 10% before the program started to about 4% today.
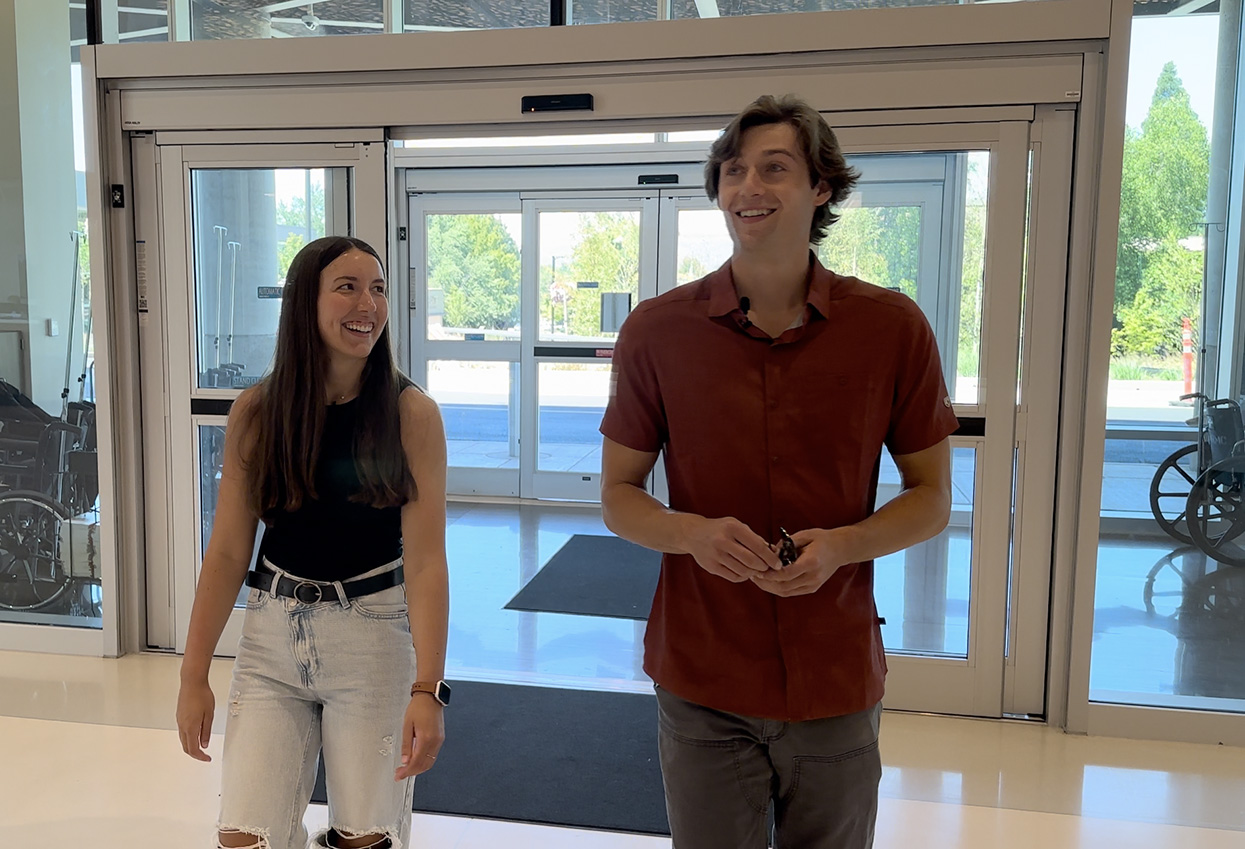
“We have one of the lowest death rates in the entire country, and that’s something we’re particularly proud of,” says Brian Gross, MD, of Southern Oregon Cardiology, who developed the program with fellow cardiologists in 2003. “The system clearly works because everybody knows their job. Everybody knows you need to move quickly.” The program is coordinated by Dr. Gross and Dr. Kent Dauterman with superb assistance by STEMI nurse Dan Moore.
The program has received the American Heart Association’s Lifeline Gold Plus STEMI Receiving award for seven years running and helped Asante Rogue Regional earn the 50 Top Cardiovascular Hospital in the nation award three years in a row.
It all began during a weekly cath conference in 2002 where cardiologists gather to review the previous week’s challenging or educational cases.
“We were frustrated by many young men and women in their 40s and 50s having a major heart attack and getting thrombolytic therapy, the established practice at the time, which involved dissolving the heart artery blood clots with intravenous medication. It only worked about 50% to 60% of the time, and in the meantime, heart muscle was dying. So we decided we were going to figure out a way to expeditiously offer stenting as a universal alternative. It was unproven, but we strongly suspected it would work. And we would offer it to every patient in our immediate catchment area of 60 miles.”
The program commenced several months later in June 2003.
“When a patient walked into an emergency room at one of the outlying hospitals with STEMI symptoms, as soon as the EKG was done, the first call would go to a paramedic unit to get the patient triaged to Rogue. The second call would be to the cardiologist on call. We were never closed for STEMI. In addition and importantly, if a patient called 911, paramedics were empowered to make the diagnosis of STEMI in the field and alert the cardiologist and team and bring the patient directly to the pre-alerted cath lab, regardless of the time of day or night. Honestly, when you have that kind of an impact on death rate, how can you ever be closed?”
The program caught the eye of the likes of the Cleveland Clinic and head of the American College of Cardiology.
When Dr. Gross attended a major strategy meeting for advancing cardiac care in 2007, hosted by Duke University at the Heart House in Washington, D.C., the opening line of the conference was, “We need to change the way we treat heart attacks across the nation. … We need to do it the way they are doing it in Southern Oregon!”
Results from Asante’s STEMI program were published in the American Journal of Cardiology and the Journal of the American College of Cardiology, and in 2009, the American College of Cardiology recommended similar protocols be established across the nation. Asante’s average “door-to-balloon time” — from the moment the patient presents with symptoms to the moment their artery is stented — is 90 minutes or less, one of the top in the nation. (Sometimes it can be as little 45 minutes if they present directly to ARRMC.)
Dr. Gross says, “I think our STEMI program serves as a model of what should happen regarding many aspects of medicine. It is a testament to what cooperation and a team-based approach can do to save or improve lives.
“You know, the paramedics, and the ER docs, and the nurses, and the cath lab crew and the other hospitals and their administrations, any one of them could have said no… and it wouldn’t have worked. It was a wonderful collaboration. It was politically and logistically challenging, but people trusted us, and now it is standard of care.”